Ethics of Precision Medicine: Mass Genotyping
- Aaron Han
- Mar 21, 2022
- 3 min read
As healthcare becomes more individualized amid the pursuit for a “magic bullet”, there may be a day when the secrets of our genome have been elucidated and shared with healthcare providers. While our personal propensities to disease and unique responses to medication does not fully lie hidden in our A, T, C, and Gs (i.e., environmental and epigenetic factors contribute similarly), our genetic information undoubtedly influences our health outcomes. How will we uncover these predictors? One possibility is to genotype the entire population at birth, which already occurs in the United States for certain genetic, metabolic, and endocrine disorders.1 Indeed, from a purely medical standpoint, mass genotyping our population is useful, ensuring that patients receive appropriate treatment. Avoiding drugs that cause allergic reactions and matching blood types during transfusions appear routine to us yet are quintessential examples of the benefits precision medicine have in our world today.

However, it is impractical to judge the merits of one aspect in a vacuum when each aspect is wholly intertwined with one another. Medicine, so central in our lives, lies at the intersection of multitudes. For one, mass genotyping compromises patient confidentiality. Are we okay with sharing so much of ourselves with clinicians, healthcare institutions, and insurance behemoths? Would we even want to know at birth our likelihood for a long and healthy life or our risk for genetic disorders? Beyond burdening people with prognoses, a future where mass genotyping is widespread could rob individuals’ feelings of autonomy, a universal psychological need that enables wellbeing.2 Ethical implementation of mass genotyping in society necessitates that a clear line be created to divide what is public and what should remain private.
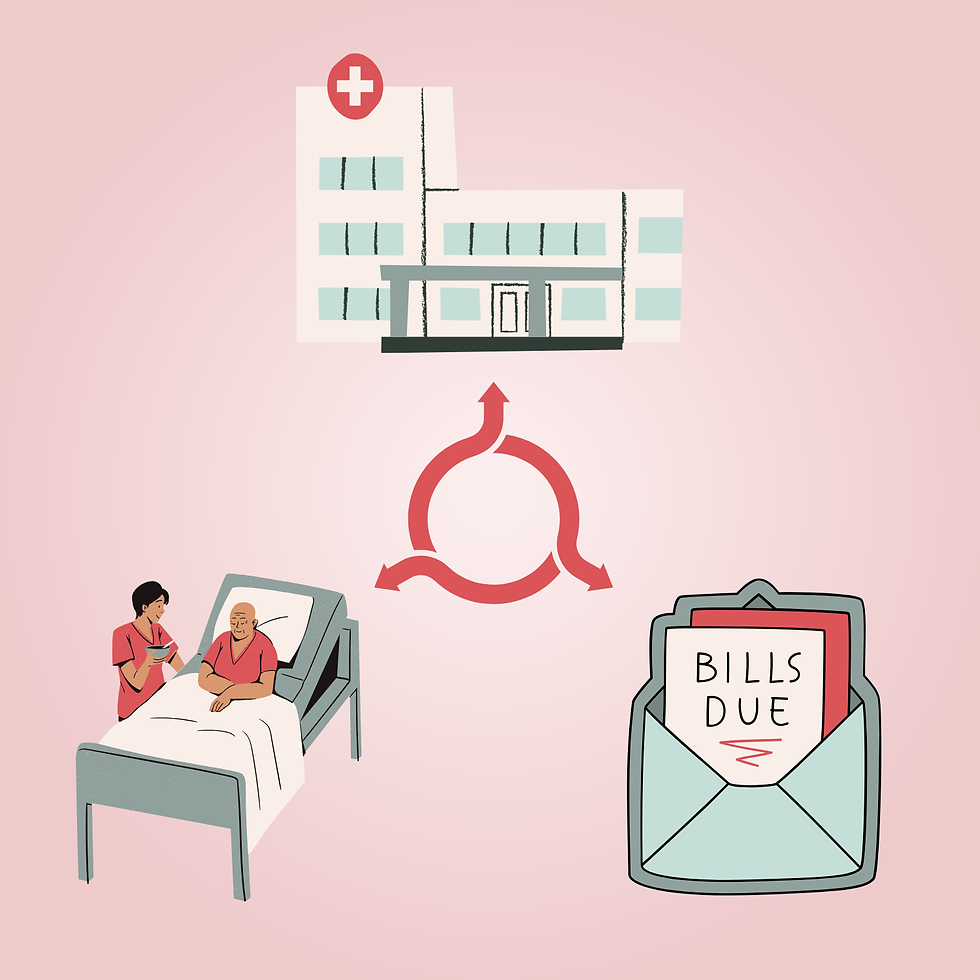
Another consideration is cost. If genotyping is neither reasonably affordable nor accessible, health disparities may worsen between higher and lower socioeconomic classes— those who can utilize it and those who cannot. Even if everyone was genotyped, different drugs may be priced differently due to supply and demand economics. This may unfairly disadvantage minority groups with rare polymorphisms if their drugs are rarer and more expensive. Additional patient information from mass genotyping may also be used by insurance companies to upcharge clients with poorer projected outcomes, which are usually those at lower socioeconomic statuses. These cost differences can all prevent social mobility and contribute to the cycle of poverty. Mass genotyping and precision medicine should be available to all, lest the chasm between classes and their health outcomes continue to widen.
When discussing genetics, race is an unavoidable topic. Despite the unscientific nature of race-based medicine (socially constructed racial groups are more genetically similar between than within subpopulations), the use of race in healthcare contributes to health disparities and reinforces institutional and individual discrimination.3 Mass genotyping may further emphasize the role genetics plays in health outcomes and add to attitudes about race-based medicine. Indeed, we have already seen the introduction of race as a biological-medical construct in the race-based pharmaceutical BiDil, which itself is mired in controversy and mixed reception.4 Nonetheless, precision medicine has the potential to transcend misconceptions about race as biologically relevant. Mass genotyping may reveal to the general public that racial groups are genetically homogenous and that human genetic variation exists most prominently from individual to individual regardless of race. Introducing precision medicine can be a powerful tool in combating racism and for promoting unity within the only race: the human race.
If precision medicine is to be used ethically and justly, society must be careful about its implementation. Stringent boundaries ought to be constructed to define what is public knowledge and what is personal information, and the remarkable benefits precision medicine can bring should be available to all. Educating the public about pharmacogenomics and social determinants of health, nebulous and complex sciences themselves, will be necessary in not only healing physical ailments, but hopefully prejudices and misconceptions as well.
Edited by: Sibani Ram
Graphic Designed by: Harris Upchurch
References:
Pitt J. J. (2010). Newborn screening. The Clinical biochemist. Reviews, 31(2), 57–68.
Yu, S., Levesque-Bristol, C. & Maeda, Y. (2018). General Need for Autonomy and Subjective Well-Being: A Meta-Analysis of Studies in the US and East Asia. J Happiness Stud 19, 1863–1882. https://doi.org/10.1007/s10902-017-9898-2
Ruqaiijah Yearby (2021) Race Based Medicine, Colorblind Disease: How Racism in Medicine Harms Us All, The American Journal of Bioethics, 21:2, 19-27, doi: 10.1080/15265161.2020.1851811
Brody, H., & Hunt, L. M. (2006). BiDil: assessing a race-based pharmaceutical. Annals of family medicine, 4(6), 556–560. https://doi.org/10.1370/afm.582


Comments